Rabies in dogs is a critical veterinary and public health concern, especially in countries with substantial stray dog populations and limited access to preventive care. Below, each heading is addressed with scientific details and unique insights from a veterinary perspective.
Table of Contents
What is Rabies in Dogs?

Rabies is an extremely fatal viral disease that affects the central nervous system, particularly the brain. It is caused by a Lyssavirus. Consider the virus as a hijacker; the virus gains entry to the body and travels through the nerves to the spinal cord and brain. Once it reaches the brain its causes severe swelling (encephalitis) that is nearly always fatal.
The most scientific fact to remember is that rabies is a zoonotic disease, meaning it can be transmitted from animals to humans. This is the main reason of rabies being a major public health concern globally.
Why is Rabies So Deadly?

Rabies is deadly due to a combination of factors:
- Neurotropism: The rabies virus has a specific affinity for nerve cells. It doesn’t travel through the blood; it slowly and silently moves along nerves fibres, effectively hiding from the immune system.
- Incubation Period: The long and variable incubation period means the disease can appear long after the bite, when it’s often forgotten.
- Lack of Effective Treatment: After the onset of clinical symptoms, there is no known cure. The disease has a near 100% fatality rate in both animals and humans.
- Misdiagnosis: Early symptoms are often flu-like and non-specific, leading to misdiagnosis until it’s too late.
Rabies in Dogs: Global & National Statistics (2024-2025 Projections)

Global statistics are sobering. According to the World Health Organization (WHO):
- Rabies causes approximately 59,000 human deaths annually, mostly in Asia and Africa.
- Over 99% of human rabies cases are caused by due to dog bites.
- 40% of people bitten by suspect rabid animals are children under 15 years of age.
- In India specifically, which carries about 36% of the global rabies burden, it’s estimated that over 20,000 people die from rabies every year.
A Critical Note on Data: Reliable and accurately reported real-time data on dog-specific rabies cases is difficult to find. The most reliable indicator of rabies burden from domestic dogs is the number of human rabies deaths because almost all (-99%) rabies deaths in humans are from dog bites. Below is a table presented with the most recent data available from global health organizations (e.g., WHO, GARC) and national reports that may provide some reflection of rabies in domestic dogs.
| Country | Estimated Annual Human Deaths (Pre-2024 Baseline) | Projected Dog Rabies Risk (2024-2025) | Key Factors & Context (from a Vet’s Perspective) |
|---|---|---|---|
| 1. India | ~20,000 (accounts for ~36% of global deaths) | Extremely High | Endemic Status. Massive stray dog population, high virus circulation, and uneven vaccination coverage keep the risk critically high. The risk remains the highest in the world. |
| 2. China | Significant historical burden, now greatly reduced. | Moderate & Declining | Successful Control Programs. Strict dog population control and mass vaccination campaigns have drastically reduced cases. Risk is now localized to specific rural areas. |
| 3. Democratic Republic of the Congo | Hundreds to over 1,000 | Very High | Limited Access to PEP. High incidence in dogs, combined with limited access to human post-exposure prophylaxis (PEP) and veterinary services, sustains transmission. |
| 4. Nigeria | Hundreds to over 1,000 | Very High | Urban & Rural Transmission. Large unvaccinated dog populations in both urban and rural settings. Lack of public awareness and coordinated control programs. |
| 5. Pakistan | Hundreds to over 1,000 | Very High | Similar Profile to India. High density of unvaccinated dogs, significant stray population, and the virus is endemic in the dog population. |
| 6. Philippines | 200-300 | High | Island Nation Challenges. Endemic in many regions. Efforts are ongoing, but logistics of mass dog vaccination across islands remain a hurdle. |
| 7. Indonesia | Hundreds | High | Archipelagic Spread. The virus is endemic in many parts of the country, particularly in areas with limited veterinary infrastructure. |
| 8. Bangladesh | Hundreds | High | High-Density Population. Intense human-dog contact in dense urban and rural areas fuels transmission, despite ongoing control efforts. |
| 9. Ethiopia | Hundreds | High | Multiple Reservoirs. Rabies is maintained in both dog and wildlife populations (e.g., jackals), complicating control efforts. |
| 10. Myanmar (Burma) | Hundreds | High | Limited Infrastructure. Challenges in implementing widespread dog vaccination and delivering PEP in remote areas maintain high transmission. |
Focus on India: Rabies in Dogs 2024-2025
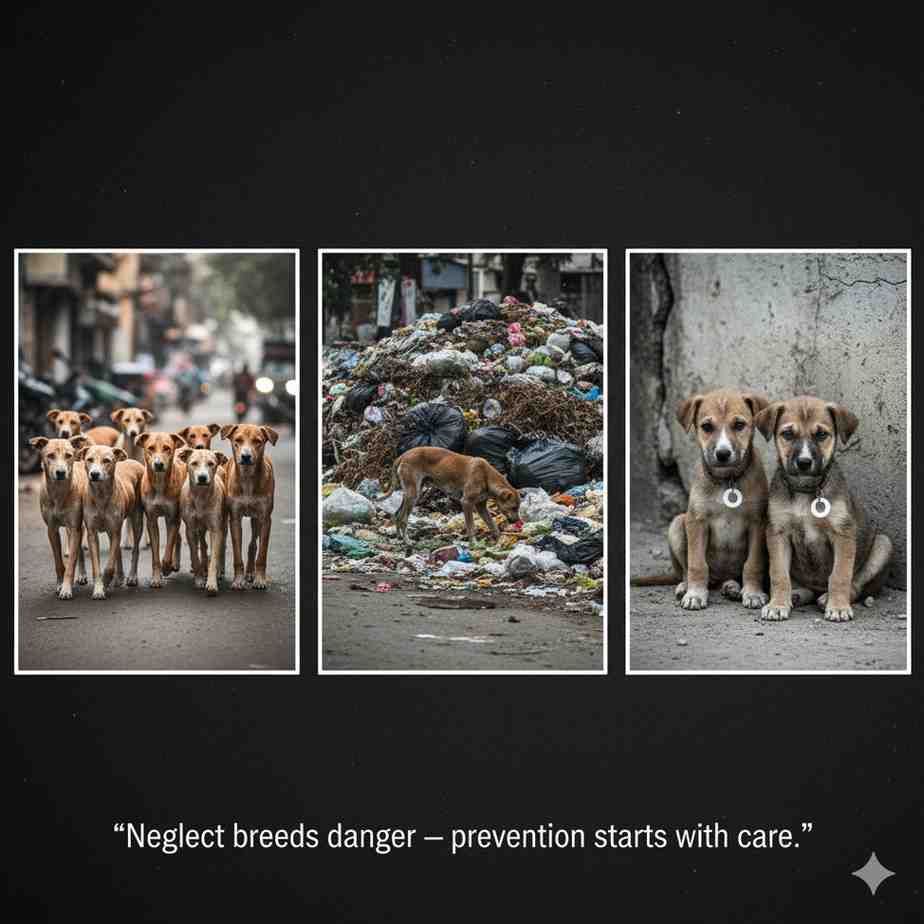
It is crucial to understand that India does not publish a official, real-time national registry for confirmed dog rabies cases. Therefore, the situation is projected based on human death data and known endemic patterns.
| Parameter | Status for 2024-2025 (Projected and Ongoing Reality) |
|---|---|
| Overall Dog Rabies Risk | Pervasively High and Endemic. The virus is continuously circulating in the massive stray and unvaccinated pet dog population. |
| Estimated Source of Human Deaths | >99% from Dog Bites. Dogs remain the principal reservoir and vector. |
| Key High-Risk Areas | Nationwide, but particularly acute in densely populated states of Uttar Pradesh, Andhra Pradesh, Bihar, and Maharashtra, and areas with low dog vaccination rates. |
| Major Contributing Factors | 1. Massive Stray Dog Population. 2. Inconsistent Dog Vaccination Coverage (falling short of the 70% WHO target in many areas). 3. Limited Public Awareness on post-bite protocols. 4. Logistical Challenges in executing pan-India animal birth control and rabies vaccination drives. |
| Positive Initiatives | Increased efforts by state governments and NGOs in Animal Birth Control (ABC) and anti-rabies vaccination drives. However, the scale of the problem means these are mitigating, not yet eliminating, the risk. |
Final Professional Assessment: During the period of 2024-2025, the risk of a dog getting rabies and transmitting the infection in India remains as among the highest globally. The statistical landscape has not changed significantly.
This underscores the non-negotiable necessity of annual or triennial rabies vaccination for every single dog, without exception. As a vet, I cannot overstate that this simple act is the most effective barrier between this fatal virus and your family.
Do All Dogs Have Rabies?
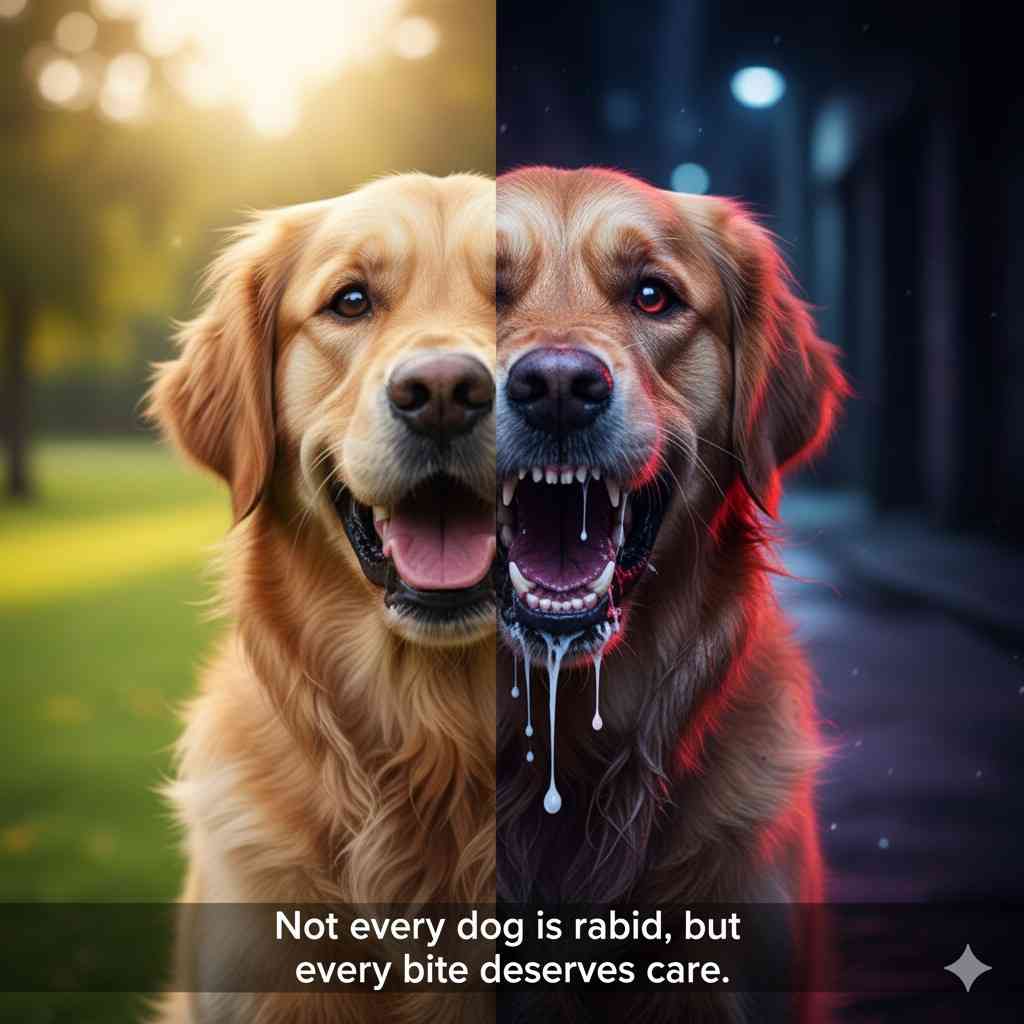
Absolutely not. This is a dangerous and incorrect misconception. However, India does have a very high prevalence of rabies in its stray dog population. It is considered a rabies-endemic country.
This means the virus is constantly circulating in the dog population. While not every dog is infected, the risk of encountering a rabid dog is significantly higher than in countries with strict vaccination and control programs. This is why vaccination is non-negotiable for any pet dog in India.
Not all dogs in India have rabies, but a large population of unvaccinated stray dogs serves as a major reservoir for the virus. While healthy, vaccinated pets are not at risk, stray and unvaccinated dogs remain the primary transmission source.
How Does Rabies in Dogs Spread?

The primary mode of transmission is through the saliva of an infected animal, most commonly via:
- Bite Wounds: This is the most common and efficient route. The virus is present in the salivary glands and is inoculated deep into tissue.
- Scratches: While less common, a scratch contaminated with infectious saliva can transmit the virus if it breaks the skin.
- Contact with Mucous Membranes: The virus can enter through the eyes, nose, or mouth if licked by a rabid animal, but this is a much rarer route of infection.
The Role of Bats in the Spread of Rabies in Dogs
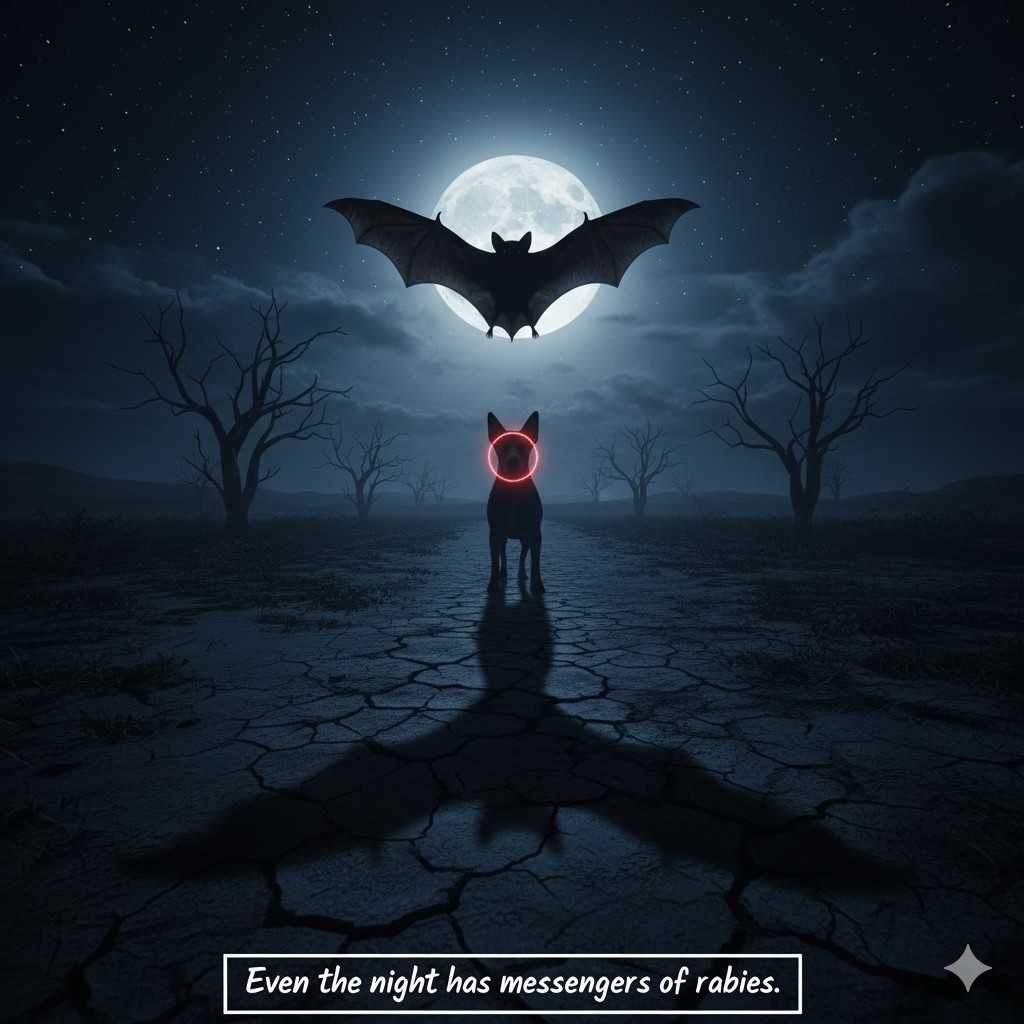
The most direct path of transmission is through interaction between a bat and a dog. This typically happens in one of two ways:
- Curiosity or Predatory Drive: Dogs are naturally curious and have a strong prey drive. A dog may find a bat that is sick, disoriented, or grounded (a common sign of rabies in bats) and:
- Bite or Mouth It: The dog picks up the bat in its mouth, attempting to play with it or kill it.
- Get Bitten: In the struggle, the rabid bat bites the dog on the nose, face, or inside the mouth.
Since the rabies virus is present in the bat’s saliva, this bite inoculates the dog with the virus, leading to infection.
- Investigation of Dead Bats: Dogs are also known to sniff, lick, or even eat dead bats. If the bat died of rabies, the virus can remain infectious in its nervous tissue and saliva for a short period. Contact with these tissues, especially if the dog has any small cuts or abrasions in its mouth or on its nose, can pose a transmission risk, although this is considered less common than a bite.
Does Every Bite Causes Rabies?
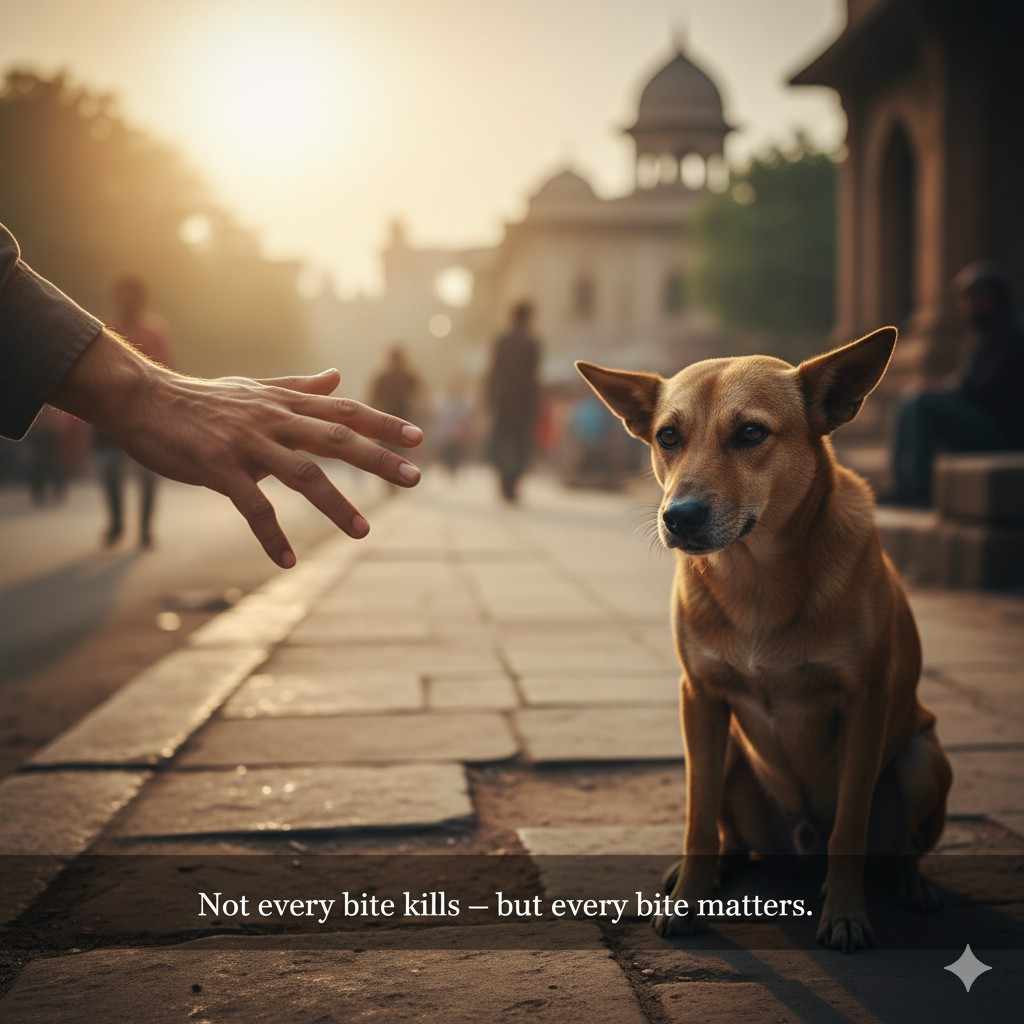
It’s a most common and understandable fear that any bite from an unknown animal will automatically lead to rabies. However, this is not the truth. For a bite to transmit the rabies virus, a specific set of conditions must be met. Think of it like this: the “chain of infection” must be unbroken for the disease to spread.
Here’s the simple explanation:
For a dog to get rabies from a bite, the animal that bit it must:
- Actually HAVE rabies at the time of the bite.
- Be shedding the live rabies virus in its saliva at the moment of the bite.
An animal only sheds the virus in its saliva during the final stages of the disease, in the days just before and after symptoms appear. A bite from a healthy animal, or an animal in the early incubation period, carries no risk of rabies transmission.
Major Factors That Are the Main Cause of Rabies in Dogs
The root cause of rabies in a dog is always exposure to the rabies virus from an infected animal. The main factors that determine this risk are:
- The first consideration is existence of rabies in the community (Reservoir Hosts) If rabies is circulating in wildlife (such as bats, raccoons, foxes, or mongooses) or in an abundant population of unvaccinated feral dogs, there is greater risk to your pet. Your dog cannot get rabies from nowhere, it has to be exposed.
- Lack of Vaccination: There is no question this is the single most important preventable cause. If a dog is not vaccinated, it is completely exposed to and completely unprotected from the rabies virus if he/she comes into contact. The vaccine is protective and protects the dog against the disease by neutralizing the virus before it ever has a chance to cause disease.
- Direct Contact with Wildlife or Stray Animals: The primary cause of infection is a dog’s interaction with a rabid animal. Common scenarios include:
- Fighting with an infected raccoon, fox, or stray dog.
- Curiosity-driven contact with a sick or grounded bat.
- Investigating a dead rabid animal.
- The Nature of the Exposure:
- Bite Wounds: Deep, severe bites, especially those on the face, neck, or close to the brain, are high-risk as they deliver a large amount of virus deep into nerve-rich tissue.
- Saliva Contact: While less common, the virus can enter through fresh, open wounds or mucous membranes (like the mouth, nose, or eyes) if licked by a rabid animal.
- Geographic Location and Local Laws: Dogs living in rabies-endemic countries (like India, parts of Africa and Asia) or regions with high wildlife rabies activity are at a much higher inherent risk. Furthermore, areas with lax vaccination laws and no effective stray animal control programs create a perfect environment for the virus to spread.
In summary: The main way rabies virus is transmitted to a dog will always stay the same, through contact of the saliva from a rabid animal, usually via a bite. The chance of this happening will change, depending on the risk of rabies in that area, and equally important, the rabies vaccination status of the dog. An area where there are rabid animals, a vaccinated dog is safer than an unvaccinated dog in an area that has little rabies risk.
Rabies Incubation Period in Dogs

The incubation period is the time from exposure to the rabies virus until the first symptoms appear. In dogs, this can range from:
- 2 weeks to several months.
- The average is 3 to 8 weeks.
This period depends on factors like:
- The location of the bite wound (bites closer to the head and brain have a shorter incubation period).
- The severity of the bite.
- The amount of virus injected.
Rabies in Dogs: Signs and Symptoms

The disease typically progresses through distinct stages. Not all dogs will show every stage clearly.
Early Signs of Rabies in Dogs (Prodromal Phase – Lasts 2-3 days)

Early signs of rabies in dogs are subtle and easy to miss. They include:
- Behavioral changes: A friendly dog may become withdrawn or apprehensive, while a normally independent dog may become unusually affectionate.
- Fever.
- Licking or chewing at the original bite site.
- Loss of appetite.
Clinical Signs of Rabies in Dogs
After the prodromal phase, the disease progresses into one of two main forms:
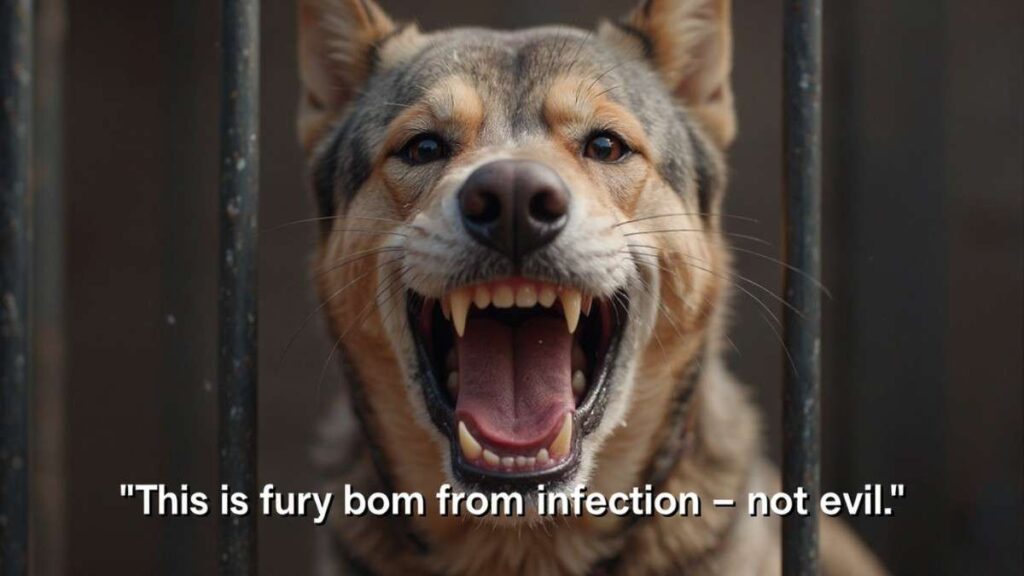
1. Furious Rabies (the “mad dog” stage)
This is the classic form of rabies virus people often imagine.
- Restlessness, pacing, and anxiety.
- Hydrophobia: Fear of water. The dog cannot swallow, so saliva drips or foams from the mouth. The sight or sound of water may cause throat spasms.
- Aggression and irritability. The dog may bite at objects, other animals, or people without provocation.
- Disorientation and seizures.
2. Paralytic Rabies (or “dumb rabies”)
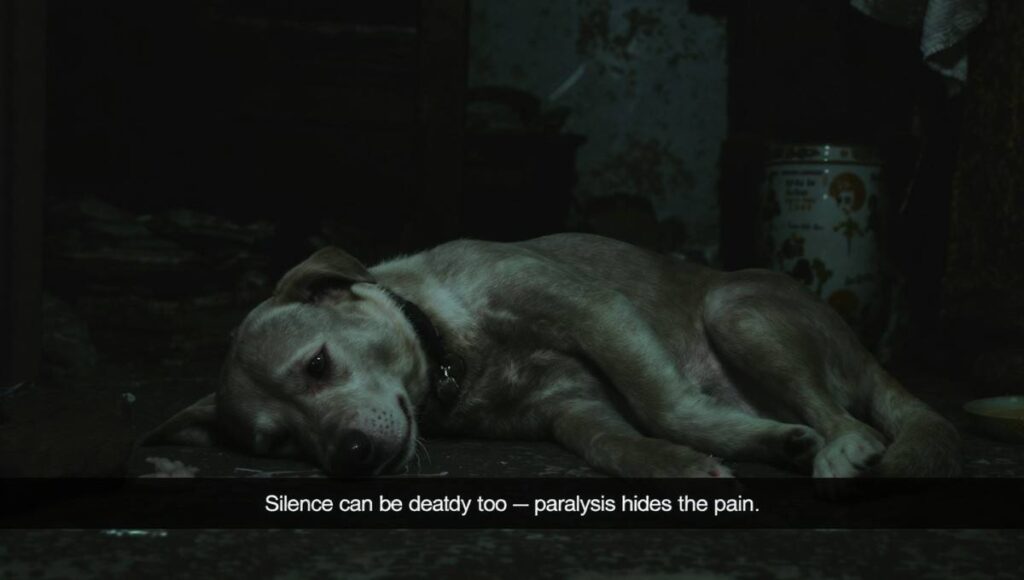
This form is more common and often misdiagnosed.
- Progressive paralysis, starting in the jaw and throat muscles.
- Dropping of the lower jaw, leading to a “dumb” look.
- Excessive drooling and inability to swallow.
- Weakness, incoordination, and eventually total paralysis and coma.
Both forms end in death, usually within 10 days of the onset of symptoms.
Asymptomatic Rabies in Dogs
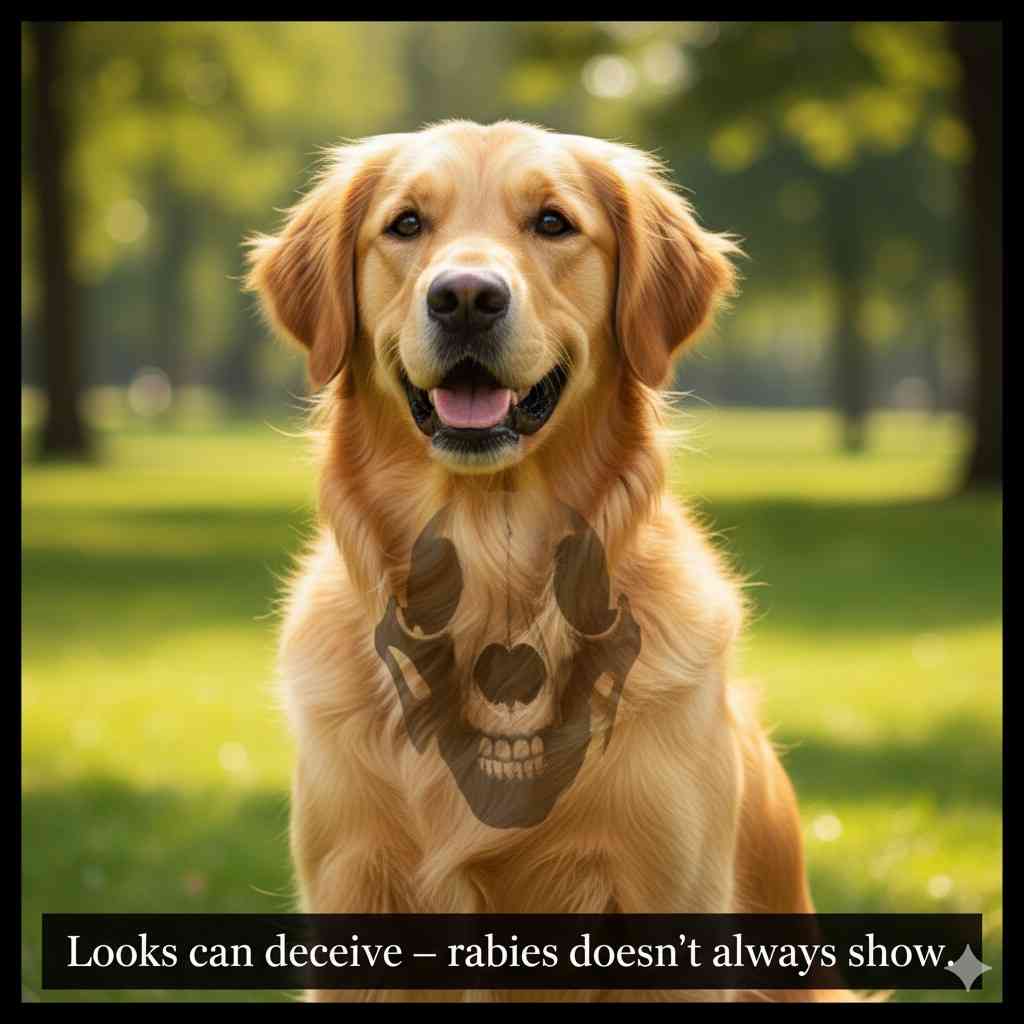
This is a critical point of confusion. A dog is not asymptomatic after the virus has reached the brain and is being shed in saliva. However, during the long incubation period, the dog will appear perfectly healthy and is not contagious.
Once a dog starts shedding the virus in its saliva (which happens in the final 1-2 days of incubation and throughout the clinical illness), it will always show symptoms, even if they are subtle. A dog that is shedding rabies virus cannot be “asymptomatic.”
Rabies in Dogs – Vaccination

Vaccination is the single most effective way to prevent rabies.
How Long Do Rabies Vaccines Last in Dogs?
Modern, killed-virus rabies vaccines are highly effective. The duration of immunity depends on the vaccine and local laws:
- Initial Vaccine: Given as a puppy, usually around 12-16 weeks of age.
- Booster: A one-year booster is typically required.
- Subsequent Vaccinations: After the first booster, many vaccines are licensed for 3 years of protection. However, always follow your local regulations, as some municipalities may require annual vaccination regardless.
WHO Rabies Vaccine Guidelines

The WHO strongly advocates for mass dog vaccination as the most cost-effective strategy to eliminate human rabies. Their guidelines emphasize:
- Vaccinating at least 70% of the dog population in at-risk areas to break the transmission cycle.
- Sustained, regular vaccination campaigns.
- The use of safe, effective, and potent vaccines.
Rabies in Dogs – Tests to Identify

There is no ante-mortem (before death) test for rabies that is reliable in a living animal. Diagnosis is confirmed post-mortem (after death) by examining the brain tissue.
Lab Test (The Gold Standard):
The Direct Fluorescent Antibody (dFA) test is performed on brain tissue to detect the presence of the virus. This is the only definitive test.
Physical “Stick Test”
This is a myth and extremely dangerous. There is no safe way to test a potentially rabid animal by poking it with a stick. Observing behavior from a safe distance can provide clues (e.g., paralysis, aggression), but it is not a diagnosis.
Would Rabies Virus Show Up In A Blood Test?
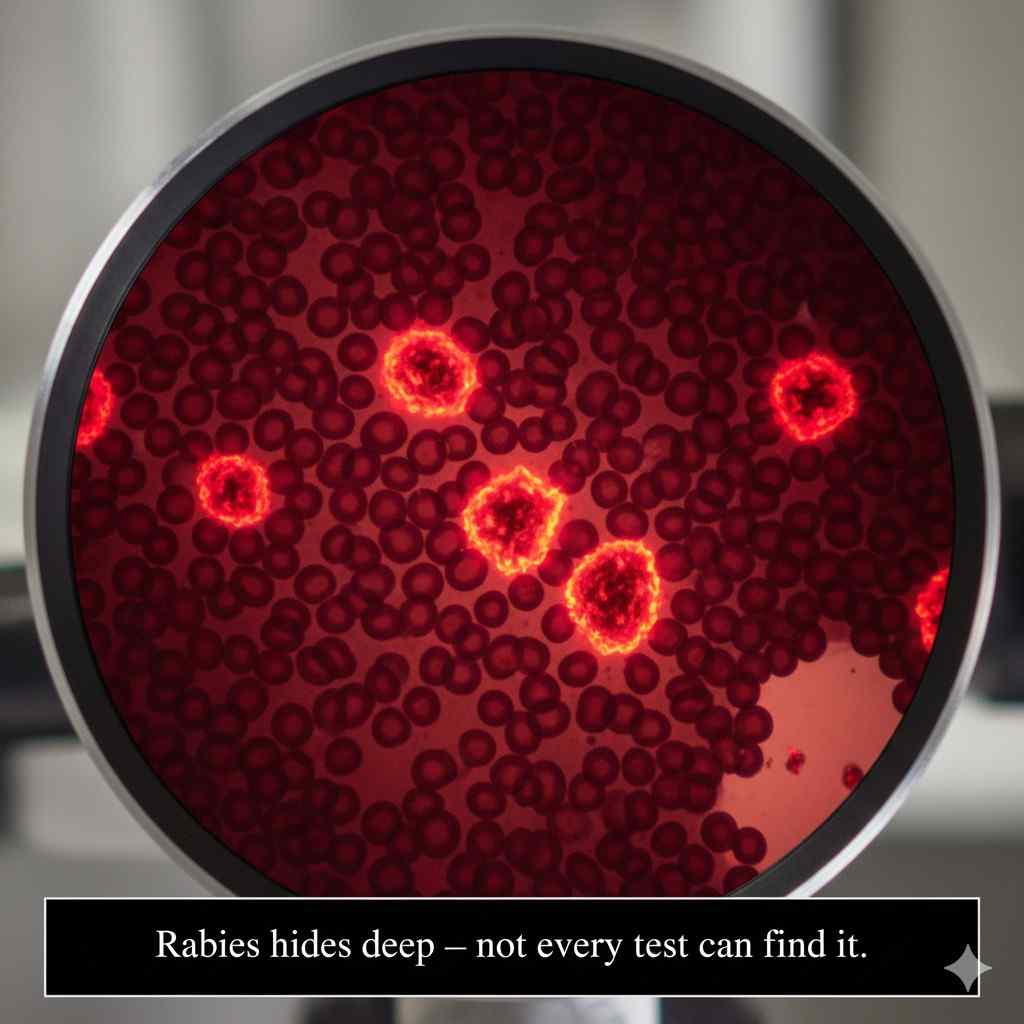
No. A routine blood test (like a CBC or chemistry panel) cannot diagnose a rabies infection. Here’s why:
- Virus Location is Key: The rabies virus is neurotropic, meaning it travels and hides within the nervous system (nerves, spinal cord, and brain). It does not circulate in large quantities in the blood.
- Immune Response is Too Late: Antibodies against the rabies virus do eventually appear in the blood, but this only happens late in the disease, often just before or after symptoms have already begun. By that time, the diagnosis is usually obvious from the clinical signs, and it is too late for treatment.
- The Gold Standard is Post-Mortem: The only way to definitively confirm a rabies diagnosis is by testing brain tissue. The required test, the Direct Fluorescent Antibody (dFA) test, can only be performed after the animal has died or been euthanized.
Important Distinction:
- Rabies Titer Test: This is a different blood test that measures the level of antibodies from a vaccine. It is used to prove a dog’s immunity for international travel, not to diagnose an active infection.
Rabies in Dogs – Prevention
Prevention is a multi-step approach:
- Vaccinate Your Pet: This is non-negotiable. Keep vaccinations up-to-date.
- Supervise Your Dog: Do not allow your pet to roam freely, especially in endemic areas.
- Avoid Contact with Wildlife: Keep your dog away from stray animals and wildlife.
- Report Strays: Report stray animals behaving strangely to local authorities.
What to Do If Your Dog Has Rabies
This is a serious emergency. Your safety is paramount.
- Do Not Approach the Dog: A rabid dog is unpredictable and can be aggressive. Do not try to handle or confine it yourself.
- Isolate and Secure: If the dog is already confined in a room or crate, do not open it.
- Call Immediately: Contact your veterinarian and your local animal control or public health department immediately. They are trained to handle such situations.
- If Bitten or Exposed to Saliva: If you, a family member, or another pet has been bitten or exposed to the dog’s saliva, immediately wash the wound with soap and running water for at least 15 minutes and seek medical attention without delay. Post-exposure prophylaxis (PEP) is highly effective if administered promptly.
The Critical 10-Day Quarantine Rule For Rabies In Dogs
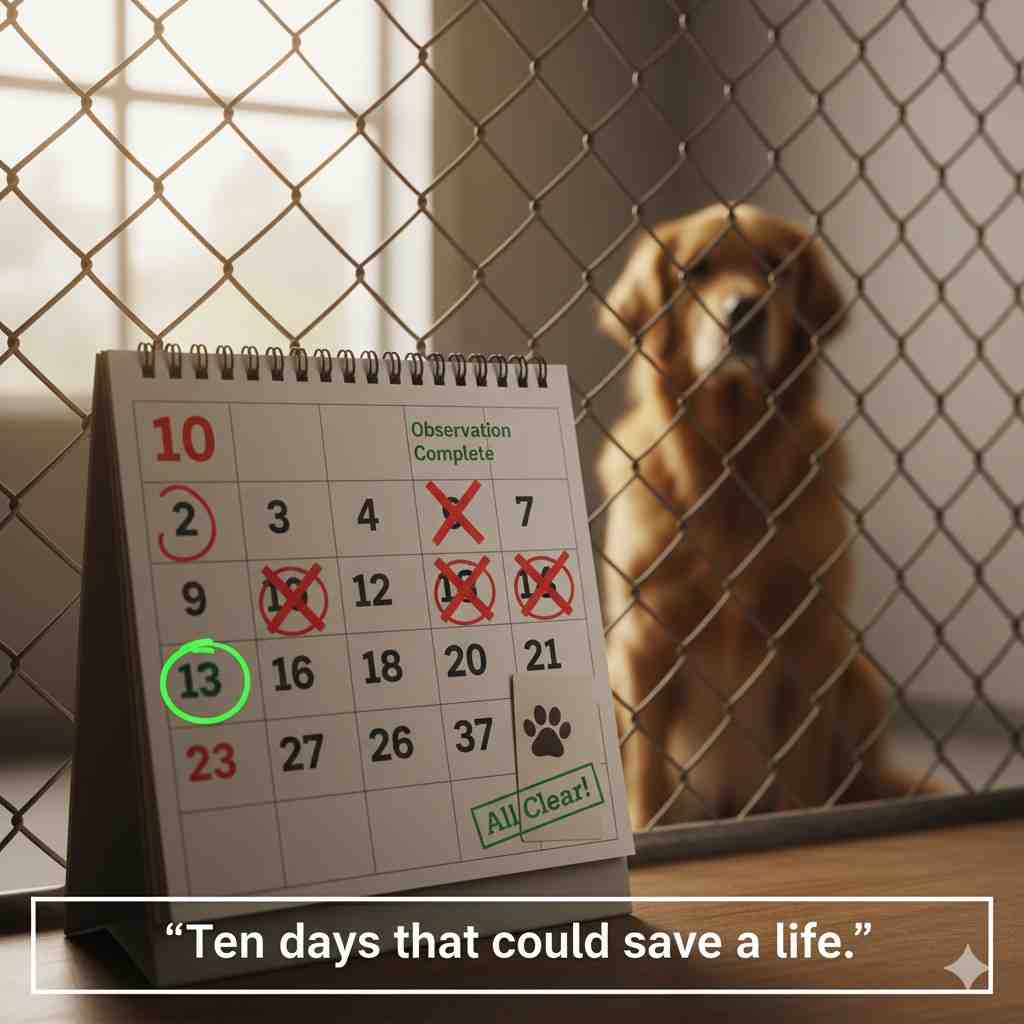
A cornerstone of rabies public health protocol is the 10-day observation period for a dog that has bitten a human.
Here’s the scientific rationale in a nutshell:
If a dog was capable of transmitting the rabies virus at the time of the bite (i.e., it was shedding the virus in its saliva), it has already reached the final stage of the infection. The progression of the virus in the body is so advanced that the animal will show clear and progressive signs of rabies, become very ill, and die within 10 days.
Therefore, if a healthy-appearing dog bites someone, it is placed under strict veterinary observation for 10 days.
- If the dog remains healthy and shows no neurological signs after 10 days, it is scientifically conclusive that it was not shedding the rabies virus in its saliva at the time of the bite. The person who was bitten does not need to undergo post-exposure prophylaxis (PEP) for rabies.
- If the dog shows any signs of rabies or dies during this period, its brain tissue is tested immediately. A positive test result would trigger the immediate start of PEP for the bite victim.
As a vet, I emphasize: This rule is a vital public health tool that prevents unnecessary medical treatment while ensuring safety. It applies only to dogs and cats, as their shedding period is well-documented. It does not apply to wildlife; a bite from a wild animal should always be considered a potential rabies exposure.
Rabies Sources: Beyond the Dog
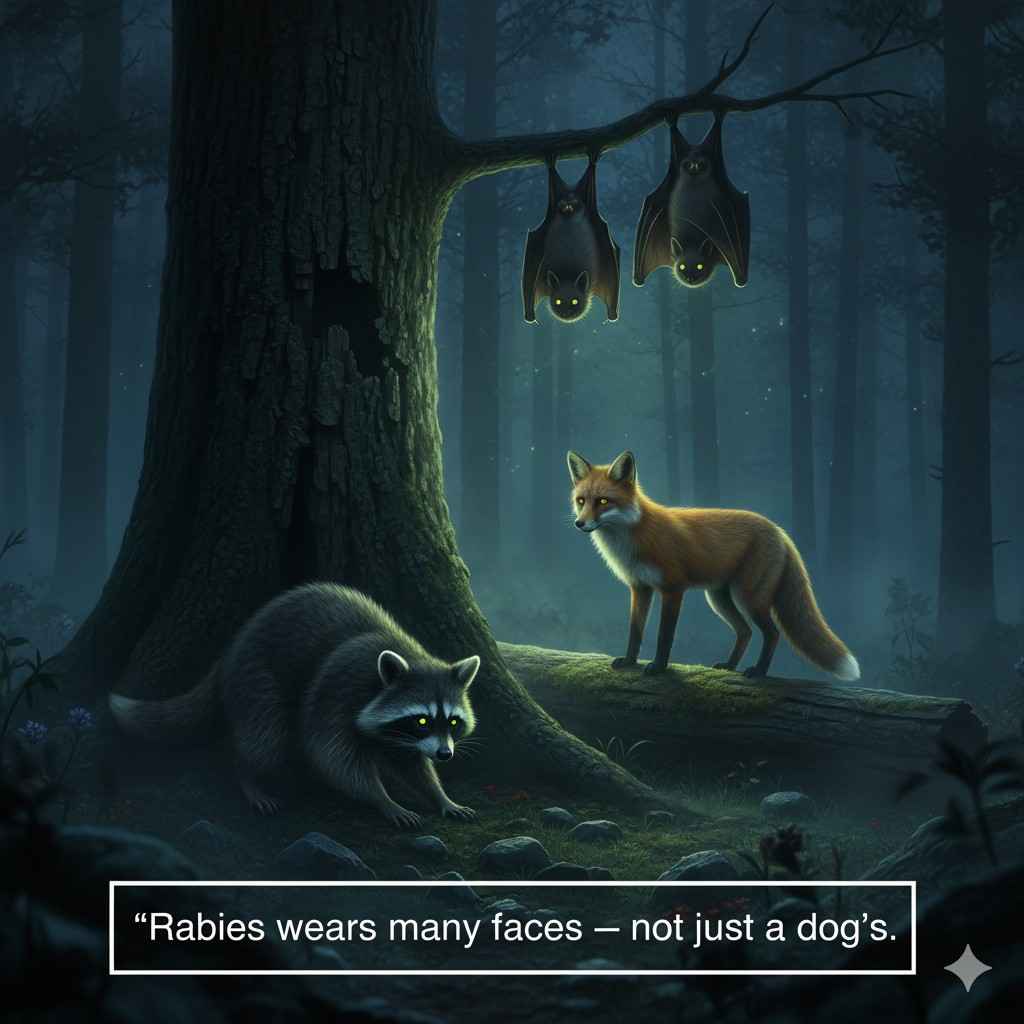
While dogs are the most common source of human rabies deaths globally, many other mammals can carry and transmit the rabies virus. These animals are known as reservoir hosts (where the virus circulates continuously in a population) or spillover hosts (infected through contact with a reservoir host).
The primary method of transmission for all species is through the saliva, almost always via a bite. The table below categorizes common animals by their role and risk.
| Animal Category / Species | Role in Rabies Virus Spread | Key Risk & Transmission Info |
|---|---|---|
| COMMON RESERVOIR HOSTS | These animals maintain and spread rabies within their species and to others. | |
| Bats | Primary Reservoir | Global risk. Bite wounds are tiny & may go unnoticed. Exposure can occur from a bite while handling a bat, or even (rarely) inhaling the virus in caves with massive bat colonies. |
| Raccoons | Primary Reservoir | High risk in North America. A common carrier known for aggressive behavior when rabid. A major threat to pets and humans due to proximity in urban/suburban areas. |
| Skunks | Primary Reservoir | High risk in North America. Known for the “furious” form of rabies, leading to bold, unprovoked aggression. Their spray does not transmit rabies. |
| Foxes | Primary Reservoir | High risk in Europe, the Arctic, and parts of North America. Red and Arctic foxes are key reservoirs. Can become unusually tame or aggressive when infected. |
| Mongooses | Primary Reservoir | High risk in Caribbean, Africa, and parts of Asia (e.g., India). A significant source of rabies in these regions, similar to the role of dogs elsewhere. |
| SPILLOVER HOSTS | These animals get infected from reservoir hosts and can transmit the virus, but typically do not maintain it. | |
| Cats | Spillover Host | Very High Risk to Humans. Due to predatory behavior, cats often encounter wildlife like bats and raccoons. Unvaccinated cats are a frequent source of human exposure. |
| Cattle | Spillover Host | Low Direct Risk. Typically get “dumb” rabies, becoming depressed and unable to swallow. They pose a risk to farmers and vets through contact with saliva during examinations. |
| Horses & Goats | Spillover Host | Low Direct Risk. Similar to cattle, they show neurological signs. Risk is through saliva exposure during handling or veterinary care. |
| Wild Animals (e.g., Coyotes, Wolves) | Spillover/Reservoir | Variable Risk. Can be infected and are dangerous due to size and aggression. Can act as reservoirs in specific localized outbreaks. |
| Monkeys | Rare Spillover Host | Low Risk. While possible, it is uncommon. Monkeys are more likely to be victims than long-term carriers. |
Final Advice As A Vet
Rabies is a tragic and fatal disease, but it is preventable. Responsible pet ownership, centered on timely vaccination, is the key to protecting your beloved dog, your family, and your community. Please, do not skip your pet’s rabies vaccine.
- Any Mammal Can Get Rabies: The list above is not exhaustive. Ultimately, any mammal, including squirrels and rabbits, can be infected, but the risk from small rodents is considered extremely low.
- Vaccinate Your Pets: This protects them from wildlife exposures and creates a crucial barrier between you and the rabid animal.
- Avoid All Contact: Never approach, touch, or feed wild animals. An animal that is unusually friendly, aggressive, or active during the day is a major red flag.
- Seek Immediate Help: If you are bitten or scratched by any wild or unknown animal, immediately wash the wound with soap and running water for at least 15 minutes and seek medical attention without delay to assess the need for post-exposure prophylaxis (PEP).
FAQs
Can a vaccinated dog get rabies?
The risk is extremely low. No vaccine is 100% effective, but a properly vaccinated dog has a very high level of protection. A booster shot is recommended after any exposure to a rabid animal.
Do all dogs with rabies foam at the mouth?
No. “Foaming” is due to paralysis of the throat muscles and excessive drooling, which prevents swallowing. This is a sign of the furious form, but some dogs get the paralytic form and just appear weak and lethargic.
Can rabies be cured in dogs?
No. There is no cure or effective treatment for rabies once clinical symptoms appear. The disease is fatal. This is why prevention through vaccination is absolutely critical.
How long can a dog live with rabies?
Once clinical symptoms begin, the disease progresses rapidly. Death usually occurs within 7 to 10 days.
Is rabies in dogs contagious to humans?
Yes, rabies is a zoonotic disease. Humans can get rabies from the bite or scratch of an infected dog. It is a major public health concern.
What should I do if my dog is bitten by a stray or wild animal?
Wear gloves to handle your dog and contact your vet immediately. Your dog will likely need a rabies booster, even if currently vaccinated. Try to safely identify the animal that bit your dog without putting yourself at risk.
How often do dogs need a rabies vaccine?
This varies by local law. After the initial puppy vaccine and one-year booster, most vaccines are effective for 3 years. However, some areas still require annual vaccination.
Can you test a living dog for rabies?
No. There is no accurate test for a living animal. A definitive diagnosis requires a post-mortem test on brain tissue.
Can a dog transmit rabies without symptoms?
No. A dog can only spread the virus when the virus has reached the brain and salivary glands, which coincides with the onset of symptoms. During the long incubation period, the dog is not contagious.
Can indoor dogs get rabies?
Yes, the risk is very low but not zero. Bats can get inside homes, and an indoor dog could escape and encounter a rabid animal. Vaccination is crucial for all dogs.
Can a small scratch from a dog cause rabies?
Yes, if the dog was rabid and its saliva contained the virus, and the scratch broke the skin. The primary route is bites, but scratches are also a risk.
Can other pets like cats get rabies?
Yes, any mammal can get rabies. Cats are actually a common source of human exposure because they are hunters and can be bitten by rabid wildlife. Vaccinating all pets is essential.
Can puppies be born with rabies?
No. Rabies is not transmitted in utero. However, a pregnant dog infected with rabies will likely pass the virus to her puppies after birth through saliva when grooming or if they are bitten.
What happens if a dog misses a rabies booster shot?
The dog is considered unprotected and vulnerable. You should contact your veterinarian immediately to restart the vaccination series. Avoid contact with other animals and wildlife until the vaccination is up-to-date.
Why does rabies cause a fear of water (hydrophobia)?
Hydrophobia is not a true fear of water, but a terrifying inability to swallow. The virus causes paralysis and severe spasms in the throat muscles. The sight or sound of water can trigger these painful spasms, making the animal avoid it.
Can my dog get rabies from a rodent (squirrel/rat) bite?
The risk is considered extremely low to negligible. Small rodents like squirrels and rats are almost never found to be infected with rabies and are not considered a reservoir for the virus.
What is the difference between a 1-year and a 3-year rabies vaccine?
The vaccine itself is often the same. The “year” designation is based on the duration of immunity proven by the manufacturer and legally recognized by local authorities. Always follow your local laws, which may require boosters more frequently than the vaccine’s scientific duration.
Can I get rabies from my dog licking me?
You cannot get rabies from a healthy, vaccinated dog. If a dog is rabid and licks an open wound, scratch, or your eyes/nose/mouth, there is a potential risk because the virus is in the saliva.
Can I travel internationally with my dog without a rabies vaccine?
No. Almost every country strictly requires a valid rabies vaccination certificate for entry. Without it, your dog will be quarantined for months or denied entry entirely. Check the specific import regulations of your destination country well in advance.
Can a dog get rabies from sharing food or water bowls?
The risk is extremely low. The rabies virus is very fragile and dies quickly once saliva dries out. However, if a rabid dog was actively drooling into a bowl and a healthy dog used it seconds later, theoretical risk exists, but this is not a documented route of transmission.
Can a dog have a reaction to the rabies vaccine?
Yes, like any medical product, reactions can occur. Most are mild and short-lived, like soreness or lethargy. Severe allergic reactions (anaphylaxis) are rare. The life-saving benefit of the vaccine far outweighs the minimal risk of a reaction.
If a rabid dog drools on a carpet, how long does the virus survive?
The rabies virus is very fragile in the environment. It is inactivated by sunlight and desiccation (drying). Once the saliva dries, the virus dies quickly, usually within minutes to a few hours. It does not persist on surfaces.
Can I get rabies from touching a dog with rabies?
You cannot get rabies from simply petting or touching a rabid dog. The virus is transmitted only when infected saliva enters your body through a bite, scratch, or fresh open wound/mucous membrane.
